Newspaper Articles About the Outcome of the Zika Virus in Babies
Abstract
Little is known well-nigh the long-term neurological development of children diagnosed with congenital Zika infection at birth. Here, we report the imaging and clinical outcomes up to iii years of life of a cohort of 129 children exposed to Zika virus in utero. Eighteen of them (14%) had a laboratory confirmed congenital Zika infection at birth. Infected neonates have a higher risk of adverse neonatal and early infantile outcomes (death, structural encephalon anomalies or neurologic symptoms) than those who tested negative: eight/18 (44%) vs iv/111 (4%), aRR 10.i [3.5–29.0]. Neurological impairment, neurosensory alterations or delays in motor acquisition are more than mutual in infants with a congenital Zika infection at nascence: half-dozen/fifteen (xl%) vs 5/96 (5%), aRR six.7 [ii.ii–twenty.0]. Finally, infected children as well have an increased risk of subspecialty referral for suspected neurodevelopmental delay past three years of life: vii/11 (64%) vs vii/51 (14%), aRR 4.four [1.9–10.i]. Infected infants without structural encephalon anomalies as well appear to have an increased risk, although to a bottom extent, of neurological abnormalities. It seems paramount to offer systematic testing for congenital ZIKV infection in cases of in utero exposure and adjust counseling based on these results.
Introduction
In the last decade, ZIKV has spread through the Pacific Islands1 and the Americasii, leading to a worldwide epidemic. Information technology is now well demonstrated that ZIKV is associated with multiple congenital abnormalities, particularly affecting the central nervous system3,4,five. Long-term disabilities, including cerebral palsy, epilepsy, and neurosensory alterations have been described in infants from the American and Brazilian cohorts6,vii,8,9. Infants included in these cohorts were by and large affected by congenital Zika Syndrome (CZS) with cerebral anomalies or neurological impairments at birth. The evolution of those with a laboratory-confirmed congenital infection but who were asymptomatic and without cerebral anomalies at birth remains poorly described. Overall, the correlation between laboratory testing for congenital ZIKV infection at birth and long-term disability including sensory and cerebral deficits is still lacking and may have major clinical and public wellness implications10.
The French Guiana Western Infirmary Center (CHOG, Centre Hospitalier "Franck Joly", referral center for western French Guiana), was confronted with the ZIKV epidemic from January to September 2016. In a previous study of a cohort of ZIKV-infected meaning women followed at the CHOG, we estimated that 279 infants were liveborn to these mothers11. Here, using a subset of these infants, nosotros prove that those with a laboratory-confirmed congenital Zika infection at nativity have college risks of imaging and clinical adverse outcomes at 2 months, 2 years, and three years of life than those tested negative at birth.
Results
Report population
Between January and September 2016, 132 newborns from 128 ZIKV-infected mothers (four dichorionic twins) were enrolled for prospective follow-up at the pediatric dispensary of the CHOG. Three of them were not tested for ZIKV earlier postpartum discharge and were excluded. Among 129 children tested for ZIKV at birth, 18 (xiv.0%) had a laboratory-confirmed congenital infection and 111 (86.0%) tested negative (details of fetal and neonatal testing are presented in Supplementary Table 1, Fig. 1 describes the enrollment).
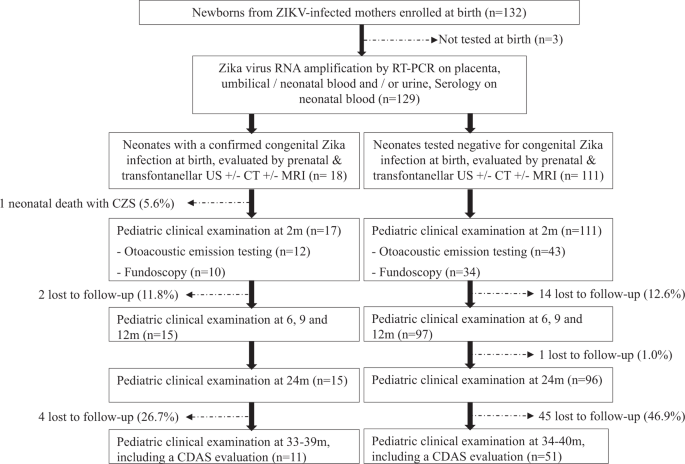
All newborns from Zika-infected mothers, living in western French Guiana and followed at the pediatric clinic of the CHOG, were enrolled in this cohort following an informed consent process. At nascence, they underwent clinical examination (including anthropometric measurements and a special focus on the neurological condition), transfontanellar ultrasound (United states of america), and testing for congenital Zika infection (PCR on urine, claret, and placenta; serology; and testing in cerebrospinal fluid if symptomatic). Later on postpartum discharge, they were recalled at 2, 6, nine, 12, 18, and 24 months of life for a pediatric exam. At 3 years of life (33–42 months), they were recalled for an evaluation of their development using the Child Development Assessment Scale (CDAS).
Baseline characteristics
Median maternal historic period at delivery was 25 and 26 years old in the group of congenital infections and the negative group, respectively. Maternal infection diagnosed in the first trimester of pregnancy was more frequent in mothers of infected newborns (38.ix% vs 24.three%). Cesarean section commitment occurred more often in these mothers (27.eight% vs 12.6%). Twins were also more frequent among infected newborns (11.one% vs 5.iv%). Alcohol and drug consumption was more frequent in mothers of newborns that tested negative for ZIKV at nascency (10.8% vs 5.half-dozen%). Other environmental or recreative exposures and co-morbidities during pregnancy including low socioeconomic condition, infant sex, charge per unit of prematurity, and neonatal accommodation were not dissimilar between these groups (Table one). Iii mothers had an identified TORCH (toxoplasmosis, rubella, cytomegalovirus, and Herpes simplex virus) co-infection during pregnancy, however, newborns tested negative during the pregnancy and at birth (i primary toxoplasmosis and two chief cytomegalovirus infections).
Neonatal and early infantile outcomes
Amongst 18 neonates with a confirmed congenital ZIKV infection at birth, 8 (44.iv%) were identified to take an agin upshot during their offset 2 months of life: 6 (33.3%) had severe structural encephalon anomalies, of whom one died in his first day of life (CZS with arthrogryposis and severe brainstem dysfunction) and two others had severe neurological symptoms. The risk of agin outcomes at 2 months was higher for infected infants compared with those tested negative at nascence (iv/111, 3.6%), even afterward adjustment for maternal infection diagnosed in the get-go trimester of pregnancy: aRR 10.1 [95% CI 3.five–29.0]. When considering only infants without structural brain anomalies, the hazard of astringent neurological symptoms was too higher in those diagnosed with a congenital ZIKV infection (2/12, sixteen.seven% vs one/108, 0.9%): aRR 20.5 [95% CI two.0–207.vii] (Table 2 and Fig. two). At two months of life, microcephaly, aberrant evoked otoacoustic emission (OAE) testing, and ocular anomalies were confirmed in ii/17 (eleven.8%), 2/12 (16.7%), and 3/10 (30%) infected infants; and in 1/111 (0.9%), 1/43 (two.3%), and 2/34 (5.9%) infants that tested negative at nascency, respectively (Table 3). Head circumference (HC) and weights, according to the results of built Zika infection testing, are presented in Fig. 3.
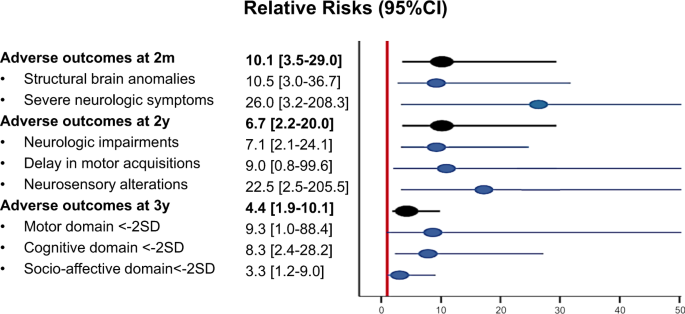
Relative risks of adverse outcomes at ii months (m), two years (y), and 3 years of life, associated with laboratory-confirmed congenital Zika infection at nativity are estimated using generalized linear models, adjusted on maternal infection diagnosed in the commencement trimester, and presented with 95% confidence intervals (95% CI). SD standard deviations.
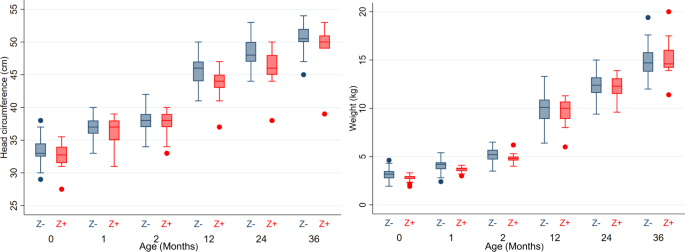
Head circumferences (in centimeters) and weights (in kilograms) are presented for each time point of this study (birth, one month, ii months, 1 year, 2 years, iii years). Boxes represent median and interquartile range (IQR), whiskers correspond range excluding outliers >1.v× IQR from upper or lower quartile, and circles represent outliers. Z-(blue): Children tested negative at birth for congenital Zika infection; Z+ (red): children tested positive at nascency for congenital Zika infection. n = 129 neonates at birth (xviii Z+/ 111 Z−), due north = 128 infants at i and ii months (17 Z+/ 111 Z−), n = 112 infants at 12 months (15 Z+/ 97 Z−), n = 111 children at 24 months (15 Z+/ 96 Z−), n = 62 children at 36 months (11 Z+/51 Z−).
Outcomes at 2 years of life
At 2 years of life, 15 children with a confirmed congenital ZIKV infection at birth and 96 who tested negative at birth were still followed at the CHOG pediatric clinic.
Amidst infected children, v/15 (33.three%) had neurologic impairments: ii with cerebral palsy, 3 with severe dystonia, and 3 with seizures. 2 of those with neurologic impairments had motor acquisition delays, fractional, or consummate blindness, and 1 had hearing deficits. Hearing impairment was also diagnosed in some other infected child, without neurologic impairments (Table 4). Overall, the risk of adverse outcomes at ii years of life was college in infected children (6/15, 40.0%) compared with those that tested negative at nascency (five/96, 5.2%), even when only considering children without structural brain anomalies (two/ten, 20.0% vs 3/93, iii.ii%): aRR 6.7 [95% CI ii.2–20.0] and aRR six.ii [1.two–33.0], respectively (Table 2 and Fig. two).
Neurodevelopment at iii years of life
Eleven (11/17, 64.7%) children of the infected group and 51 (51/111, 45.ix%) children of the group that tested negative at birth presented for neurodevelopmental screening in August and September 2019. The median age at evaluation was 35 months in the infected group and 36 months in the group of children that tested negative at birth. A developmental score below −2SD ("Referral" zone) in at to the lowest degree 1 domain was observed in vii/11 (63.vi%) infected children, the cognitive and language domain being the most affected (vi/11, 54.5%). Details of the Child Development Assessment Scale (CDAS) are presented in Table iv and Fig. 4. Children with a confirmed congenital ZIKV infection at birth had a higher risk of a CDAS score in the "referral zone" (<−2SD) compared with children that tested negative (7/51, 13.7%), fifty-fifty when considering but those without structural brain anomalies: aRR four.4 [one.nine–10.1] and aRR 3.0 [1.0–ix.0], respectively (Tabular array 2 and Fig. 2).
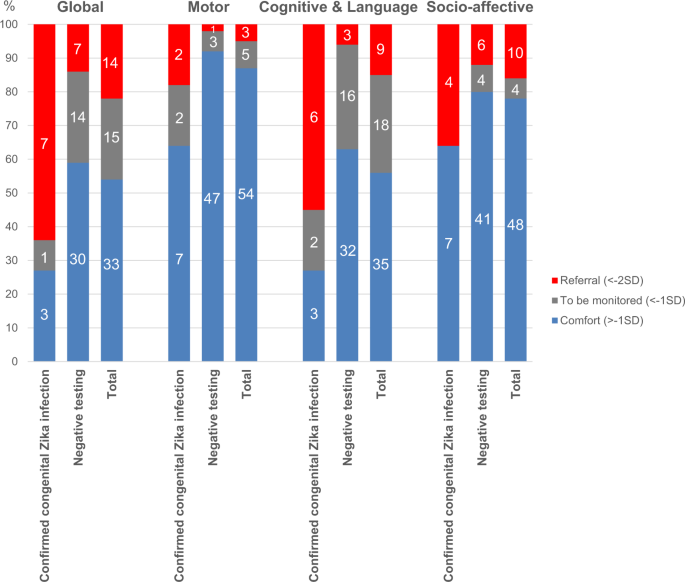
All children followed for in utero ZIKV exposure were recalled for a developmental evaluation using the Child Development Cess Scale at iii years of life (33–42 months, due north = 62). Normal results are classified in the "comfort" or "blue" zone (>−1 standard deviation [SD]). Intermediate results are classified in the "to exist monitored" or "grayness" zone (−2SD; −1SD). Suspicion of delays is classified in the "referral" or "red" zone (<−2SD). The motor, socio-emotional, and cognitive & linguistic communication domains were evaluated using this calibration. Results of these domains were synthesized in a global evaluation.
Children with a CDAS score in the "referral zone" were the same who had an adverse outcome at two years among the infected. In addition, one infected babe without structural brain anomalies and who remained asymptomatic until ii years of historic period was screened equally at take chances for developmental filibuster at 3 years of life.
Event-modifiers
Exposures during pregnancy, maternal historic period, co-morbidities, socioeconomic condition, infant sexual activity, twins, prematurity, and the mode of delivery were tested as effect-modifiers on main outcomes, and no interactions were identified. The presence of structural brain anomalies, all the same, was an upshot-modifier for severe neurological symptoms at 2 months of life, and on adverse outcomes at two and three years of life. A sub-analysis of children with and without structural brain anomalies is presented in Table 2.
Discussion
Main results
In this study, nosotros assessed the development of children with laboratory-confirmed congenital ZIKV infection up to iii years of age. Our results signal that infected neonates have a higher risk of neurological symptoms at birth (27.eight%), fifty-fifty when no structural encephalon anomalies are observed (16.7%), as compared with neonates that tested negative at birth (0.9%). At 2 years of age, infection at birth was still associated with a college risk of neurologic impairment and/or neurosensory amending (40.0% vs 5.2%). At iii years of life, suspicion of neurodevelopmental delay (<−2SD) was more common in children that tested positive at birth (63.6% vs 13.seven%). All those that tested positive at birth and had structural brain anomalies had evidence of neurodevelopmental delay (<−2SD) (iv/iv), compared with less than half in those without structural brain anomalies (three/7).
Interpretation
Structural brain malformations and ocular anomalies associated with congenital Zika infection have been well described worldwide, particularly in CZSv,7,12,thirteen,fourteen,xv,xvi. Developmental outcomes of infants exposed to ZIKV in utero have been studied less extensively, often lacking stratification by infant ZIKV infection status at birth. The study by Nielsen-Saines and colleagues identified similar findings to us including abnormal neurodevelopmental and/or ophthalmological or auditory assessments in 31.5% of children evaluated betwixt 7 and 32 months of age17. In this study, the cognitive and language domain was as well the about affected (35% of 146 children). When comparing neuroimaging findings to neurodevelopmental functioning in ZIKV-exposed infants, Lopes Moreira et al.half dozen noted a significant clan betwixt normal results on brain imaging and higher Bayley-III scores. Yet, they failed to predict severe developmental delay in ii% of children and normal development in 16%. Similarly, in our cohort overall (i.e., regardless of ZIKV infection condition at birth), ~twenty% (10/56) of the children without structural brain anomalies had evidence of neurodevelopmental filibuster in at least i domain at 3 years of life, whereas i-3rd (ii/vi) with brain anomalies did not. The results of the Colombian cohort reported by Mulkey et al.18 point that neurodevelopmental delay in a child that is healthy at birth could worsen with age.
Brasil et al.19 performed a study stratifying infants by their ZIKV infection status at nascence. They described neurodevelopmental outcomes of 130 children born to ZIKV-infected mothers, of whom 84 (65%) tested positive for ZIKV between nascence and i year of historic period. They could only observe trends towards an association betwixt laboratory-confirmed infection and specific abnormalities (structural brain anomalies, vision and hearing deficits, abnormal neurological exam, developmental delay). The disparity betwixt their results and ours may be explained by the difference in testing strategy for congenital infections, as a positive result after postpartum belch is not able to differentiate congenital infections from post-natal caused infections. Every bit a result, a potentially higher proportion of exposure misclassification may have biased their estimates towards a zippo clan.
The impact of the trimester of maternal infection is contradictory in some studies. In the cohort from Rio de Janeiro, the authors found that agin outcomes were non correlated with the trimester of maternal infection3. Other cohorts take identified higher rates of brain structural anomalies and CZS in cases of maternal infection in the first trimester4,16,20. In our study, we observed a higher proportion of infants with neonatal, early infantile, or agin outcomes at 2 and 3 years of life after maternal infection diagnosed in the showtime trimester of pregnancy, although this divergence was not meaning as our study does non appear to be sufficiently powered to conclude on this covariate (Supplementary Table iii). Moreover, our study reports the trimester at infection diagnosis but does not permit to accurately date maternal infection, as the diagnosis is based on serology in many cases.
Overall, the results from our study along with those from previously published studies seem to point that a laboratory-confirmed congenital ZIKV infection at birth could be associated with higher risks of long-term outcomes, fifty-fifty in children without structural brain anomalies. As a normal antenatal and neonatal evaluation cannot provide complete reassurance for children exposed to ZIKV in utero, it seems paramount to offering systematic testing for congenital ZIKV infection at birth in cases of in utero exposure and to conform counseling according to these results.
Study limitations
The get-go limitation of this study is the proportion of individuals lost to follow-up reducing the sample size from 129 to 111 later on ii years and to 62 later on three years and introducing a potential selection bias. Loss to follow-up is critical in determining a study's validity equally patients lost to follow-upwardly might have a different outcome than those who complete the study. In our study, although not pregnant, the proportion of loss to follow-up was higher amongst children who tested negative at nascency compared with those with a confirmed congenital infection (threescore/111, 54.1% vs vi/17, 35.3%, p = 0.1494, Std diff = 0.38), which suggests a potential selection bias on the result. Yet, it is hard to know if the loss to follow-upward has selected the more astringent cases or not. 1 would argue that the lack of clinical concern by parents, particularly in asymptomatic cases, might accept driven the loss to follow-up. This would have overestimated the absolute risks of infantile adverse outcomes and the suspicion of neurodevelopment filibuster in the accomplice, specially in those that tested negative at birth. Thus, absolute risk in this study should be considered carefully.
Another source of potential option bias is linked to practical limitations for follow-up at the CHOG for newborns from mothers living along the Maroni River or in isolated areas in Suriname. Among the newborns born at the CHOG, merely those that would be followed at the CHOG pediatric clinic were enrolled, resulting in the exclusion of 35% of the CHOG-born newborns from ZIKV-infected mothers, leading to the initial inclusion of simply 129 infants. This might have selected infants stemming from families with a college socioeconomic condition. This would have led to a possible underestimation of the absolute risk although unlikely as this choice impacted both groups.
The 2nd limitation of this study is the testing performance to confirm congenital infections. In fetuses and neonates, it has been demonstrated that viremia is transient in blood, amniotic fluid, and urine21. Thus, the window to detect congenital infections using reverse transcription-polymerase concatenation reaction (RT-PCR) may exist shorter than for other built infections (i.east., CMV). In infants, built ZIKV infections are difficult to ostend retrospectively, attributable to serological test cantankerous-reaction and the possibility of infection after nativity in the context of continuous exposure. To avoid false-negative or false-positive results, neonatal serology was performed earlier postpartum discharge. As no other flaviviridae was circulating significantly during this menstruation, we considered the risk of cross-reactions depression, and a positive neonatal IgM without positive RT-PCR was considered as a laboratory-confirmed built infection, although these would be considered equally probable cases per CDC definitions22. Nosotros tried to reduce the gamble of misclassification biases by performing neonatal testing on unlike samples (Appendix i), yet, we cannot exclude that some newborns classified equally uninfected had undetectable viremia and immune response at birth. To increase the sensitivity of neonatal testing, we included positive RT-PCR on placental samples in the definition of laboratory-confirmed congenital ZIKV infections23. Withal, we did not observe contradictory results in cases of infected placentas, as all also had a positive IgM and/or RT-PCR in fetal/neonatal samples.
The follow-upward of infants and children was based on the French recommendations24 and adapted to local capacities, but nosotros cannot exclude that routine MRI, auditory brainstem response testing, and consultation with a pediatric neurologist, as recommended past the CDC, would have diagnosed more than subtle and specific signs of congenital ZIKV infection.
The tertiary limitation is the presence of a language barrier. Some children or mothers accept difficulties when using the French language. These difficulties could have wrongly led to a lower score when using the French version of the CDAS to evaluate the cognitive & language domain, resulting in misclassification of the outcome. The two practitioners who evaluated these children, however, were also able to speak the local language and translate questions, limiting the poor understanding of the CDAS assessment. This would accept led to an overestimation of the difficulties in the cerebral and linguistic communication domain, however, this issue would likely have impacted both groups equally.
The concluding limitation was that a command group of children built-in from uninfected mothers who underwent neurodevelopmental testing using the CDAS was not bachelor. In the full general population, a normal distribution of neurodevelopmental scores would be expected when using a standardized tool such every bit the CDAS, only this test has never been used in French Guiana and cerebral scales, in particular, may include items that could be influenced by the cultural context. In a cross-sectional report evaluating the neurodevelopment of Polynesian infants built-in during the ZIKV outbreak versus a command grouping of Canadian infants, Subissi et al.25 described that misreckoning factors such equally socioeconomic status and cultural factors may play an important role in infantile neurodevelopmental assessment.
Methods
Study settings and participants
This prospective cohort study included newborns from mothers infected with ZIKV during pregnancy that were followed at the CHOG after the 2016 ZIKV epidemic. The CHOG offers the only maternity and neonatal intensive care units in western French Guiana. During the ZIKV epidemic (January to September 2016), all meaning women in the territory underwent laboratory screening by ZIKV serology in each trimester and at commitment, too as RT-PCR in urine and plasma samples for those with symptoms.
All infected women were followed in the fetal medicine unit of the CHOG. Fetal ultrasound (US) examinations were performed every 3–4 weeks using E8 and E10 Voluson scanners with abdominal (RM6C) and transvaginal (RIC5-9-D) transducers (General Electric Healthcare, Zipf, Republic of austria). Additional investigations (MRI, computed tomography (CT), amniocentesis) were performed based on U.s.a. results and after a discussion with a multi-disciplinary team. All neonates from ZIKV-infected mothers living in the area (Fig. five) were offered ongoing follow-up at the CHOG until the third year of life and participation in this study. Asymptomatic neonates from mothers living along the Maroni River, outside of the Saint-Laurent du Maroni area, were discharged with their mother subsequently 24-hour interval 3–5 postpartum and were followed in the nearest principal healthcare center, and merely returned to the CHOG in cases of emergency or demand for advanced care. Thus, these infants were not included in this cohort.
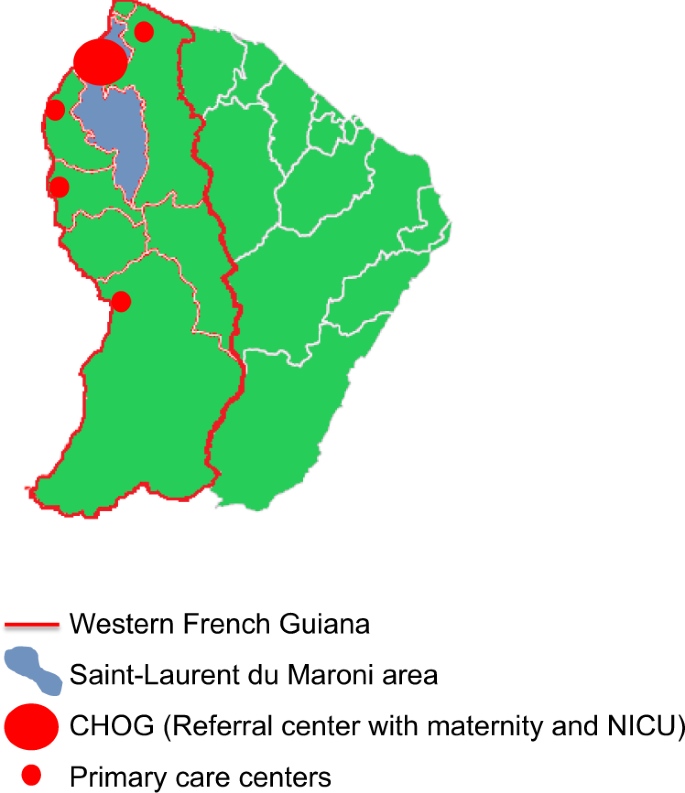
All newborns from Zika-infected mothers, living in western French Guiana (within the red lines) and followed at the pediatric dispensary of the CHOG (large red dot), were enrolled in this cohort. Asymptomatic neonates from mothers living outside of the Saint-Laurent du Maroni area (bluish area), were discharged afterward day iii–5 postpartum and were followed in the nearest principal healthcare center (modest scarlet dot).
The study received ethics approving from the institutional review board of the CHOG and written consent of the mother was obtained.
Laboratory testing for congenital ZIKV infection and exposure definition
During pregnancy, RT-PCR on amniotic fluid was offered for cases with fetal anomalies or if an amniocentesis was performed for another indication (i.e., aneuploidy diagnosis). Afterward birth, all newborns underwent ZIKV serology for detection of specific IgM earlier mean solar day three of life. RT-PCRs were performed in cord claret, neonatal urine, and placenta. Boosted testing on cerebrospinal fluid was proposed in cases with neurological symptoms or demise.
Nosotros defined a laboratory-confirmed congenital ZIKV infection either past positive RT-PCR from at to the lowest degree 1 fetal/neonatal sample (amniotic fluid, cerebrospinal fluid, urine, blood, placenta) or identification of specific IgM in neonatal claret or in cerebrospinal fluid.
Neonates from ZIKV-infected mothers without a confirmed congenital ZIKV infection were classified as controls.
Molecular and serologic testing was performed at the French Guiana National Reference Eye for arboviruses (Institut Pasteur of French Guiana, Cayenne, French Guiana) using the Realstar Zika Kit (Altona Diagnostics GmbH, https://altona-diagnostics.com) for RT-PCR, and in-house enzyme-linked immunosorbent assay (ELISA) and IgM antibody-capture (MAC) ELISA for serologic testing. The limit of detection for serum samples tested using the Realstar Zika Kit was 0.61 (95% CI 0.39–1.27) copies/μL, and a bicycle threshold value <37 was considered positive. The following primers were used: (1) ZIKV 1086 1086–1102 CCGCTGCCCAACACAAG; (2) ZIKV 1162c 1162–1139 CCACTAACGTTCTTTTGCAGACAT; (3) ZIKV 1107-FAM 1107–1137 AGCCTACCTTGACAAGCAGTCAGACACTCAA. ELISA and MAC-ELISA testing was based on whole virus antigens, with a positive result divers as 3 standard deviations higher up the negative control value. Its sensitivity for specific IgM detection was estimated at 98% after solar day 7 from symptoms onset in an developed cohort26.
Details of maternal, fetal, and neonatal testing are available in our previous studies4,11. Placentas were sampled and tested according to the method described in our dedicated report, which also corresponds to what was proposed by Seferovic and colleagues23,27.
Consequence definition and fourth dimension of measurement
Newborns underwent cerebral imaging and neurosensory testing and were followed by a pediatrician up to 3 years of life. The terminal evaluation included a neurodevelopmental screening using the CDAS28.
Neonatal and early infantile outcomes
All ZIKV-exposed neonates, regardless of their testing result at birth, underwent clinical examination with special attention to anthropometric measurements, neurological status, and signs of infection. The HC measurements were confirmed 24 h after birth to avoid the effects of commitment sequelae. In addition to clinical examination, they were assessed by transfontanellar Usa, hearing evaluation by OAE testing, and fundoscopy (1–2 months afterward nativity). Every abnormal examination was reconfirmed, and more investigations (MRI, CT) were requested depending on the clinical movie.
Neonatal and early infantile adverse outcomes were divers as neonatal death (between birth and 2 months of life, intrapartum demise not included), structural brain anomalies, or astringent neurological symptoms (according to Pomar et al., BMJ, 2018; Prenat diagnosis, 2019)11,29.
Follow-up and outcomes at 2 years of life
All infants enrolled were scheduled for medical consultation at the CHOG pediatric clinic at 2, 6, 9, 12, 18, and 24 months of life. These pediatric examinations included parental questioning on baby development, anthropometric measurements, assessment of motor acquisition, a neurological examination, and an auditory and visual assessment, post-obit the French loftier Quango of Public Wellness (HCSP) recommendations24.
Agin outcomes at two years of life were defined as the ascertainment of neurologic impairment (cerebral palsy, astringent dystonia, tremors, or seizures), motor conquering filibuster (sitting position >9 months or walking >18 months of historic period), or neurosensory alterations (impaired response to visual or auditory stimuli) until the age of 24 months.
Neurodevelopmental outcomes
In August and September 2019, at 3 years of life, the children were screened for neurocognitive development using the French version of the CDAS28. Adapted to children 0–v years of age, the results allow the user to evaluate the kid's cognitive, language, motor, and social-emotional development using a validated and standardized scale. Results in the "comfort zone" (blueish, >−1SD) betoken normal development. Results in the "to be monitored zone" (gray, [−2SD to −1SD]) suggest that interventions with the kid should be adapted according to identified difficulties and that the child should exist reassessed later. Finally, results in the "referral zone" (red, <−2SD) indicate that the child should be referred for an exhaustive developmental cess. To avert any bias of administration, all children were evaluated by two medical doctors trained to perform the CDAS test and blinded for the results of congenital Zika infection testing.
A suspected filibuster in neurodevelopment was divers every bit a CDAS below −2SD ("referral zone") in at least one domain at 3 years of life.
Mitigation of bias
In the context of French Guiana, infants have an increased risk of loss to follow-upwardly later on postpartum belch, every bit some alive in isolated areas and are followed in primary care centers. These infants were not included in the accomplice to avoid misclassification bias. In infants enrolled in the cohort, when missed appointments occurred, the parents were recalled to schedule another evaluation. We did not enroll infants referred to the CHOG for advanced intendance who were not included initially in the cohort, to avoid selection biases.
OAE testing was implemented in May 2016 and infants built-in before that fourth dimension were non systematically tested at birth. Later the epidemic peak, we encountered human and technical limitations to perform fundoscopy in all children born from ZIKV-positive mothers. To avoid selection and classification biases, we did not consider abnormal fundoscopies or OAE in primary outcomes. Instead, we considered an abnormal response to auditory or visual stimuli in infancy, as all the infants were tested for these outcomes.
Statistical analysis
Baseline characteristics of mothers and newborns were obtained at enrollment and presented every bit absolute and relative frequencies for those diagnosed with a laboratory-confirmed congenital Zika infection at nascence and those that tested negative. Timing of maternal infection diagnosis was estimated based on symptom onset or on laboratory results in cases of asymptomatic infection; and grouped into first or second and third trimesters for the analysis. Gestational age at nascence was considered as a binary variable for the assay ("prematurity < 37 wg").
Standardized differences were calculated to compare baseline characteristics of patients with laboratory-confirmed congenital ZIKV infection at birth to those who tested negative. These characteristics were considered unbalanced when the standardized difference was >0.1.
The relative risks (RR) associated with laboratory-confirmed congenital ZIKV infection were assessed using generalized linear models, and were adjusted (aRR) for confounding factors (trimester at maternal ZIKV infection diagnosis), and controlled for potential interactions with exposures during pregnancy, maternal age, co-morbidities, and socioeconomic status, infant gender, twins, prematurity and the style of delivery. Structural brain anomalies were also tested equally effect-modifiers for astringent neurological symptoms, adverse outcomes at 2 years of life, and suspicion of neurodevelopmental delay < −2SD. In the case of interaction, the analysis was stratified for effect-modifiers.
We performed a complete example analysis, thus using unlike denominators for outcomes at 2 months, 2 years, and 3 years of life.
Data were collected using Excel software and analyzed using Stata 15 (Stata Corporation, College Station, TX, U.s.).
Reporting summary
Further information on research design is bachelor in the Nature Inquiry Reporting Summary linked to this article.
Data availability
Source data that underlie the results are provided with this paper (supplementary information). Other individual participant data volition be shared with researchers who provide a methodologically sound proposal for the multicentric written report, particularly individual participant data meta-analysis. Proposals should be directed to leo.pomar@chuv.ch. Source data are provided with this newspaper.
Code availability
The codes used in Stata 15 software to clean, analyze and present Tables one–4 are provided with this newspaper ("Supplementary Codes").
References
-
Haddow, A. D. et al. Genetic characterization of Zika virus strains: geographic expansion of the Asian lineage. PLoS Negl. Trop. Dis. half-dozen, e1477 (2012).
-
Brasil, P., et al. Zika virus outbreak in Rio de Janeiro, Brazil: clinical label, epidemiological and virological aspects. PloS Negl. Trop. Dis. 10 (2016).
-
Brasil, P. et al. Zika virus infection in pregnant women in Rio de Janeiro. N. Engl. J. Med. 375, 2321–2334 (2016).
-
Pomar, L. et al. Association between Zika virus and fetopathy: a prospective accomplice study in French Guiana. Ultrasound Obstet. Gynecol. 49, 729–736 (2017).
-
Moore, C. A. et al. Characterizing the blueprint of anomalies in congenital Zika syndrome for pediatric clinicians. JAMA Pediatr. 171, 288–295 (2017).
-
Lopes Moreira, Chiliad. E. et al. Neurodevelopment in infants exposed to Zika virus in utero. N. Engl. J. Med. 379, 2377–2379 (2018).
-
Satterfield-Nash, A. et al. Health and development at age 19-24 months of 19 children who were born with microcephaly and laboratory bear witness of congenital zika virus infection during the 2015 Zika Virus outbreak - Brazil, 2017. MMWR Morb. Mortal. Wkly Rep. 66, 1347–1351 (2017).
-
Rice, M. E. et al. Vital signs: Zika-associated nascency defects and neurodevelopmental abnormalities peradventure associated with built Zika virus infection - U.South. territories and freely associated states, 2018. MMWR Morb. Mortal. Wkly Rep. 67, 858–867 (2018).
-
Alves, L. V., Paredes, C. E., Silva, Yard. C., Mello, J. G. & Alves, J. G. Neurodevelopment of 24 children born in Brazil with congenital Zika syndrome in 2015: a case series study. BMJ Open 8, e021304 (2018).
-
Honein, Thou. A., Woodworth, K. R. & Gregory, C. J. Neurodevelopmental abnormalities associated with in utero Zika virus infection in infants and children-the unfolding story. JAMA Pediatr. 174, 237–238 (2020).
-
Pomar, L. et al. Maternal-fetal transmission and adverse perinatal outcomes in significant women infected with Zika virus: prospective cohort study in French Guiana. BMJ 363, k4431 (2018).
-
Johansson, M. A., Mier-y-Teran-Romero, Fifty., Reefhuis, J., Gilboa, S. M. & Hills, S. L. Zika and the risk of microcephaly. N. Engl. J. Med. 375, ane–4 (2016).
-
Yepez, J. B. et al. Ophthalmic manifestations of congenital Zika syndrome in Colombia and Venezuela. JAMA Ophthalmol. 135, 440–445 (2017).
-
de Paula Freitas, B., et al. Ocular findings in infants with microcephaly associated with presumed Zika virus congenital infection in Salvador, Brazil. JAMA Ophthalmol. 134, 529–535 (2016).
-
Sanz Cortes, M. et al. Clinical cess and encephalon findings in a cohort of mothers, fetuses and infants infected with ZIKA virus. Am. J. Obstet. Gynecol. 218, 440 e441–440 e436 (2018).
-
Hoen, B. et al. Pregnancy outcomes after ZIKV infection in French territories in the Americas. N. Engl. J. Med. 378, 985–994 (2018).
-
Nielsen-Saines, K. et al. Delayed childhood neurodevelopment and neurosensory alterations in the second yr of life in a prospective accomplice of ZIKV-exposed children. Nat. Med. 25, 1213–1217 (2019).
-
Mulkey, S. B., et al. Neurodevelopmental abnormalities in children with in utero Zika virus exposure without congenital Zika syndrome. JAMA Pediatr. 134, 529–535 (2020).
-
Brasil, P. et al. Zika virus vertical manual in children with confirmed antenatal exposure. Nat. Commun. 11, 3510 (2020).
-
Shapiro-Mendoza, C. K. et al. Pregnancy outcomes after maternal Zika virus infection during pregnancy - U.S. territories, Jan 1, 2016-Apr 25, 2017. MMWR Morb. Mortal. Wkly Rep. 66, 615–621 (2017).
-
Schaub, B. et al. Analysis of claret from Zika virus-infected fetuses: a prospective example series. Lancet Infect. Dis. 17, 520–527 (2017).
-
Adebanjo, T. et al. Update: interim guidance for the diagnosis, evaluation, and management of infants with possible built zika virus infection - United States, October 2017. MMWR Morb. Mortal. Wkly. Rep. 66, 1089–1099 (2017).
-
Seferovic, M. D., et al. Clinical importance of placental testing among suspected cases of built Zika syndrome. Int. J. Mol. Sci. 20, 712 (2019).
-
HCSP. Avis relatif à la prise en charge médicale et au suivi des nouveau-nés et nourissons ayant été exposés au virus Zika in utero ou présentant une infection congénitale à virus Zika (2017).
-
Subissi, L. et al. Zika virus infection during pregnancy and furnishings on early babyhood development, French Polynesia, 2013-2016. Emerg. Infect. Dis. 24, 1850–1858 (2018).
-
Flamand, C., et al. The proportion of asymptomatic infections and spectrum of affliction amongst pregnant women infected by Zika virus: systematic monitoring in French Guiana, 2016. Euro Surveill. 22, 17-00102 (2017).
-
Pomar, L., et al. Placental infection by Zika virus in French Guiana. Ultrasound. Obstet. Gynecol. https://hal-pasteur.archives-ouvertes.fr/pasteur-02863590 (2019).
-
CLIPP. The Child Development Assessment Scale: a scientifically validated tool (2010).
-
Pomar, L., et al. Zika virus during pregnancy: from maternal exposure to built Zika virus syndrome. Prenat. Diagn. 39, 420-430 (2019).
Author information
Affiliations
Contributions
N.H. conceived and designed the written report, provided care to mothers and children, collected the information, and typhoon the initial manuscript. Y.K. and Z.H.50.R. provided intendance to children, collected data, and reviewed and revised the manuscript. V.Fifty., K.M., and G.C. participated in the written report blueprint, provided care to mothers, collected information, and reviewed and revised the manuscript. D.B. and A.P. analyzed and interpreted the data, and reviewed and revised the manuscript. L.P. conceived and designed the report, provided care to mothers, analyzed and interpreted the data, and drafted the initial manuscript. All authors approved the final manuscript as submitted and concur to be answerable for all aspects of the work.
Respective author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional data
Peer review information: Nature Communications cheers Kjersti Aagaard and the other, anonymous, reviewer for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher'southward notation Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This commodity is licensed under a Creative Commons Attribution 4.0 International License, which permits employ, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(southward) and the source, provide a link to the Creative Commons license, and point if changes were made. The images or other third party material in this article are included in the article's Creative Eatables license, unless indicated otherwise in a credit line to the material. If fabric is not included in the article'south Artistic Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you volition demand to obtain permission straight from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/past/4.0/.
Reprints and Permissions
About this article
Cite this article
Hcini, N., Kugbe, Y., Rafalimanana, Z.H.L. et al. Association betwixt confirmed congenital Zika infection at birth and outcomes up to 3 years of life. Nat Commun 12, 3270 (2021). https://doi.org/10.1038/s41467-021-23468-3
-
Received:
-
Accustomed:
-
Published:
-
DOI : https://doi.org/10.1038/s41467-021-23468-3
Comments
By submitting a comment you concord to abide past our Terms and Customs Guidelines. If you find something abusive or that does not comply with our terms or guidelines delight flag information technology as inappropriate.
Source: https://www.nature.com/articles/s41467-021-23468-3
0 Response to "Newspaper Articles About the Outcome of the Zika Virus in Babies"
Post a Comment